|
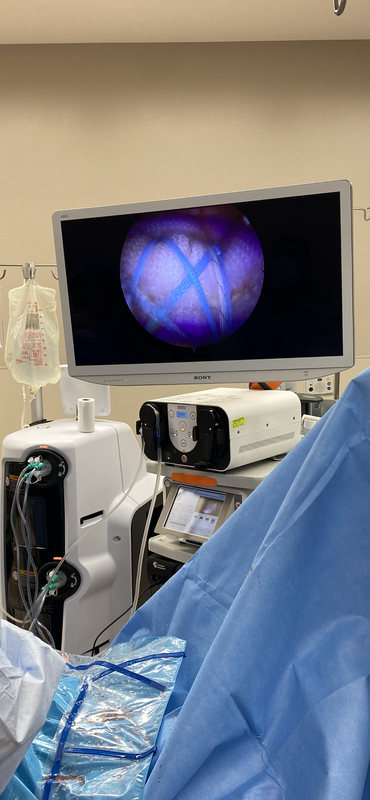
I became aware of Biorez because of Linkdin. For several months, I dismissed it as “just another patch” until I saw Scott Sigman MD and Shariff K. Bishai, DO on there posts. The reality of a bioinductive and structural augmentation may be a huge advancement in rotator cuff surgery (and other soft tissue surgeries). I’m not the first in Texas but who can beat Don Buford, MD in the biologics race. Yesterday, I implanted three, revision supraspinatus (below), retracted subscap and a revision distal triceps. Now for the tough part of any new procedure or product, it’s time to start tracking the outcomes and determining it’s place in the algorithm of care.
#Biorez #Biobrace #biologics #rotatorcuff #structural
0 Comments
I may not have posted in almost 5 years but the business of shoulder surgery hasn't stopped moving forward and neither have I. My belief is that I should never stop striving for improvement in my practice of shoulder surgery for the sake of my patients. As a result, I continue to read about and learn new procedures. I've had some changes to my practice including the addition of JT Matthews, NP over 3 years ago who is an invaluable part of my clinical team. We have also added multiple new procedures, listed here:
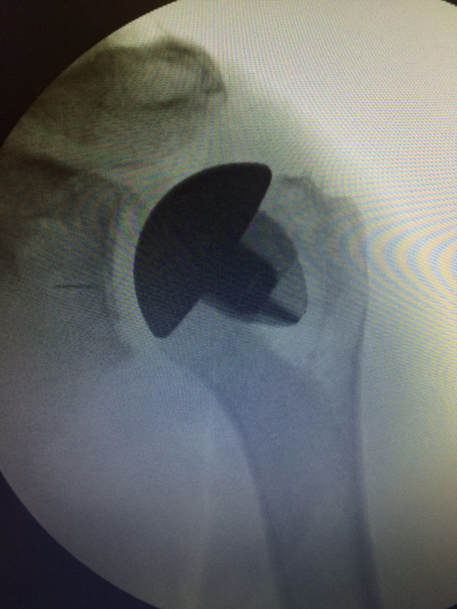
1. Scope Assisted Lower Trapezius Transfer 2. Latissimus Dorsi tranfer for subscapularis insufficiency Combo of 1 and 2 being called a Parachute Procedure for massive irreparable anterior, superior and posterior cuff tears 3. Arthroscopic Pectoralis Minor release for STAM 4. Custom Glenoid baseplates for severe glenoid deformity or revision setting 5. Significant increase in use of BIO-RSA (up to 25-30% of my RSA practice) and occasional use of femoral head allograft for oversized defects, instead of custom baseplate. 6. Utilization of inset glenoid technology in conventional shoulder arthroplasty 7. Arthroscopic Anterior Glenoid Reconstruction for severe anterior glenoid bone loss 8. Improved Blueprint preoperative planning 9. New inlay humeral stem from Stryker/Tornier for more anatomic RSA design 10. Utilizing APC allografts with Lower trapezius transfer for humeral bone loss situations (2 cases coming up this month with this technology) I am sure there are more that I haven't listed here. The bottom line is that there have been huge advancements in a relatively short period of time and this an exciting time to practice shoulder surgery. If your shoulder surgeon is doing the same surgeries the same exact way he/she was 5-10 years ago, it may be worth taking a second look. I will always have more to learn and improvement to be made, but the first step is recognizing that this art is not perfected. New innovations in orthopedic surgery continue, but nowhere as quickly as shoulder arthroplasty. In the last 2-3 years, the FDA has cleared the first canal sparing, sometimes called the stemless shoulder replacement, the Wright/Tornier Simpliciti shoulder arthoplasty system. This company has also been responsible for the development of augmented glenoids (shoulder sockets) for defects and problems that had previously been very difficult to reconstruct. Finally, Wright/Tornier along with the software company, Imascap, developed a software program based on CT scans for surgical preplanning and intraoperative guidance. As a conservative surgeon, I was not one of the first adopters of the canal sparing design. I wanted to see results and proof before using this technology on my patients. That proof came from some of the best shoulder replacement surgeons in the country and the world, and I was convinced. It took less prodding to start using the Blueprint planning software. I attended the Tornier Masters course about two years ago in Minnesota and had several lectures touting this technology. It makes good sense that going in with a plan is better than having no plan at all. The fate was sealed after speaking with Gilles Walch, a world renowned French shoulder specialist. I admire the French for a couple of things in particular, bordeaux wines and advancements in shoulder surgery. He is legendary in France. At my home, we jokingly refer to Dr. Walch as a shoulder surgery god! He developed the Blueprint software but said that even if he had not, he would use it in every single case. My decision was made. If a "shoulder god" could be a better surgeon with this technology, my patients and I would benefit even more. These two pieces of metal and the software that was used to create them can make your surgeon 10 times more accurate. Who wouldn't want that? Those surgeons that use preplanning are likely to be more accurate even without the 3D printed guides than those who do no preplanning. The larger chunk on the left is a 3D metal printing of the socket and the smaller piece on the left is the guide that fits to the glenoid in surgery to place the guide pin in the correct position and angle. With this, the guide pin variance in position is less than 1 mm and the angle variance in any direction is approximately 1 degree versus 10-11 degrees without the guide. I get my hands on the glenoid before I ever cut the skin. Yes, that is my thumb. For those wondering, it is brachydactyl type D, a common thumb difference affecting a small percentage of the population. Nevertheless, I get to feel and experience the defects of the socket before surgery. The second smaller hole on the guide is an antirotation drill hole. It is designed for use with augmented glenosphere to ream the portion of the socket that needs to be augmented. This patient had 25 degrees of tilt of his glenoid, 0-8 degrees is normal. If this isn't corrected, the shoulder replacement will fail much more quickly. This xray is the culmination of all three technologies and in my opinion the very best that I or anyone else could have offered the patient. We were able to anatomically restore the shoulder alignment with thorough planning and new augmented socket designs and use a canal sparing implant which in my experience has resulted in less pain postoperatively for the patient.
My goal for all of my patients is to do the best, most conservative treatment. If that is surgery, I will use all the best new innovations at my disposal to perform the best, longest lasting surgery possible. Today and July the 27th were two days that I have both dreaded and highly anticipated for the last nine years. July 27th was seeming culmination of my orthopedic training into two hours of oral examination. I was happy to have that day behind me after 9 months of preparation and 9 years of hearing how bad it was. Today was the pay off, the email that you've been dreading/buzzing about for the last month. A positive outcome, indeed. I must thank God, my wife, family, staff at Scott and White, Dr. John Itamura, all of the examiners at the ABOS, and those that offered thoughts and prayers on my behalf.
As a disclaimer, the videos and photos before and after are two different patients that have given permission to have their images posted. The patient in the "after" video is a young man injured in military training several years ago. He had failed physical therapy and had EMG findings consistent with a long thoracic nerve palsy causing medial scapular winging. It is clear to see that the scapula does not move correctly. Pardon the sideways video. The second video shows a "scapular compression test" illustrating better forward elevation with compression of the shoulder blade against the chest wall. A portion of the patient's pectoralis tendon was disconnected from the humerus, routed along the chest wall and attached to the lower border of the shoulder blade. In the video below, the patient is about 10 weeks postop. His function is drastically improved from his preoperative function and continues to improve. He has returned to full duty. Family is one of the most important aspects of my life as I have noted on this website. It is important to know where you come from and who you represent. In my life, I represent the Kummerfeld family values, work ethic, etc. In my work, I represent those who have been responsible for my training directly or indirectly. My training in orthopedics at Scott and White was invaluable, but I will focus on the family tree of my specialty training in shoulder and elbow surgery. A physician's training cannot make them great, but it instills potential for knowledge, experience, and skill which can combine to make a competent physician. I am proud of my family tree in orthopedic surgery. Here is my lineage linking back to the father of shoulder surgery.  John Itamura, my shoulder dad Doctor Itamura is my mentor in shoulder and elbow surgery. He is responsible for teaching me most everything I know within the specialty. He is known in California and the western US as one of the "go to" surgeons for complex and revision surgery of the shoulder and elbow. I have noted Grandpa Kummerfeld's role in me ending up with Dr. Itamura at the Kerlan Jobe Clinic.  Buz Burkhead, my shoulder granddad Doctor Burkhead is a well known shoulder surgeon in Dallas, Texas at the Carroll Clinic. He taught John Itamura about complex shoulder and elbow surgery. In addition to this teaching, Burkhead taught Dr. Itamura about Texas (cowboy boots, cowboy hats, country music, and everything else great about Texas). Among other honors, he is a past president of the American Shoulder and Elbow Surgeons. His training came through a fellow Texan a few hours south on I-35. I am privileged to know him personally and professionally.  Charles Rockwood, father of Texas shoulder surgery Doctor Rockwood is responsible for training many great Texas shoulder surgeons including Dr. Burkhead. He has been a fixture at UT San Antonio for several decades teaching residents and fellows about life and shoulder surgery. I have not had the pleasure to meet him personally, but have heard exemplary things about him as a man and a surgeon. He is also a past president of the American Shoulder and Elbow Surgeons. Doctor Rockwood was one of the original fellows of Charles Neer, a prominent figure in orthopedics and the father of shoulder surgery.  Charles Neer, father of modern shoulder surgery Doctor Neer is one of the great innovators in orthopedics surgery. He is directly or indirectly responsible for many advances in shoulder surgery and the training of the orthopedists responsible for these advances. In his training, he was dissatisfied with the outcomes of fracture treatment of the shoulder. As a result, he created one of the first(if not the first) mass produced shoulder replacements in history. I will never have the opportunity to meet Dr. Neer as he passed away in 2011, but will be ever grateful for the family of surgeons that has been responsible for my orthopedic training and upbringing. It is important to know who you are and where you come from, as well as who your doctor is and how they were trained. I am proud of this tradition of excellence and hope to make my predecessors proud as I care for my patients. Grandpa Kummerfeld My grandfather is one of the reasons why I pursued shoulder surgery. In addition to being someone who helped instill in me a solid work ethic via my father, he was also the example of someone who required expertise and a special skill set when it came to his shoulder problems.
He has always been a very active man. He is one of those people that seems to know how to do everything. Even if he didn't, he wasn't going to let anyone know that. As a child, I remember that he was always busy with projects and work that he and his family were typically the labor force. When he wasn't working, he was spearfishing, pole fishing, or going on adventures in Baja California. A kink was thrown in the works when he had his right shoulder replaced while living in Long Beach, CA. It was never quite right. Admittedly, he did more than someone with a total shoulder should do, but that's just being a Kummerfeld. Even though things weren't great with his shoulder, he pushed through it. Again, that's just being a Kummerfeld. He eventually gave in and was referred to John Itamura, a shoulder and elbow specialist at USC at the time. He had an initial surgery revising the total shoulder that functioned well for several years, but became clear that something hadn't been right from the start. It turned out that he had a latent infection, likely from the very beginning, that caused things never to feel quite right. He one surgery to clear the infection and one more to reconstruct his shoulder with a bone graft and reverse total shoulder. Meeting Dr. Itamura was the best thing that happened to my grandpa's shoulder and was pretty fortunate for me too. As a result of what transpired, I was able to meet with Dr. Itamura in San Francisco in 2012 at the Academy of Orthopedic Surgery meeting and interview for his fellowship. I was accepted and spent August of 2013-July 2014 learning how to manage problems just like my grandpa's shoulder. I can say with certainty that I wouldn't be the man I am without my grandfather and I wouldn't be the surgeon that I am without the tutelage of John Itamura. It was a fun, grueling, tiring, exciting and transformative year. Thanks to that experience, I can bring that knowledge and insight back to the people of East Texas to care for their shoulder and elbow ailments. I have been in Tyler a year and 2 months, finally finished with a rigorous medical training in Orthopedic Surgery and shoulder and elbow fellowship training. Tyler is definitely different than Los Angeles, but mostly good ways. I am biased being Texan, born and raised, spending my formative years in Tyler where my family settled after my father finished his cardiology training and became the third heart specialist in Tyler in 1984. It's great to be back in town, practicing my craft, and most importantly helping people feel better.
My time in Los Angeles was invaluable. My mentor, John Itamura, is a great teacher and a great man. He holds a special place in our family as my grandfather's shoulder surgeon, my mentor and a friend to my girls. He taught me the finer points of shoulder surgery, including things I thought I may never need to know. It turns out East Texas has its own surprises. I've needed just about every tool in my first year that he equipped me with during that year of specialty training. From being proficient in simple shoulder and elbow arthroscopy to complex revision replacement surgeries, rare muscle transfers about the shoulder and even shoulder fusions, I've seen it all here in my hometown. I'm so thankful the Dr. Itamura and God's Providence in preparing me for what East Texas has had to offer. I am also fortunate that I am surrounded by specialists in my own group. As a young orthopedist, I see everything and can treat most things. At Azalea Orthopedics, I have the luxury of being able to refer to a number of partners that specialize in just about every joint in the body. I am blessed to be able to care for people's shoulder and elbow needs, blessed by my community and family and very happy to be back home doing what I have a passion for. I tell my girls all of the time that whatever they do, they should strive to be excellent. That is my goal in all areas of my life but especially caring for those that entrust themselves to me. I have been trained in excellence and intend to practice excellence. |
AuthorOrthopedic Shoulder and Elbow Surgeon back in his hometown to practice Archives
August 2022
Categories |







 RSS Feed
RSS Feed